Plantar Fasciitis and Heel Spurs
Plantar fasciitis is a common foot problem in athletes, especially runners. It starts as a dull intermittent pain in the heel which may progress to a sharp persistent pain. Typically, it is worse in the morning with the first few steps, after sitting or standing, or at the beginning of a sport or activity.
The plantar fascia is a thick fibrous material on the bottom (plantar aspect) of the foot. The fascia is attached to the heel bone (calcaneus), extends forward toward the toes, and acts like a bowstring to maintain the arch of the foot.
Anatomy

The Injury
Plantar fasciitis usually occurs when part of this inflexible fascia is repeatedly placed under tension, as in running. Repeated tension or overload of the fascia causes inflammation at its attachment point to the heel bone. The inflammation produces pain.
Plantar fascia injuries can also occur at the midsole or near the toes. Since it is difficult to rest the foot, the problem gradually worsens and is aggravated with every step. In severe cases, the heel is visibly swollen. The problem may progress rapidly, and treatment must be started as soon as possible.
If the chronic overload causes the fascia to pull away from the heel bone, then the foot reacts by filling in the space with new bone. This new formation results in the heel spur. The heel spur sometimes shows on X-rays. Heel spurs do not cause the initial foot pain, nor do they cause the problem. Heel spurs are a result of the problem. Later on, walking on a foot with a heel spur may cause sharp pain.
Contributing Factors
- Flat (pronated) feet
- High-arched, rigid feet
- Improper shoes with inadequate support
- Toe running and hill running
- Soft terrain (i.e., running on sand)
- Increasing age
- Sudden weight increase
- Sudden increase in activity or training level
- Family tendency
Treatment
Improvement and pain relief may take longer than expected, especially if the condition has existed for a long time. As the injury begins to heal, the athlete should return to full activity gradually.
RICE.
Which stands for rest, ice, compression, and elevation.
REST. The degree of rest will depend on the severity of the inflammation. The athlete may have to temporarily stop running or playing his sport to allow the injury to heal. Continuing the sport or activity often aggravates the injury, causing the athlete to experience pain, possibly more than initially. The athlete should use pain as his guide. Once pain begins to subside, foot exercises can be started to improve flexibility, allowing the athlete to resume his sport sometime in the future.
ICE. Ice (e.g., bag of ice) can be applied to the foot for 20 – 30 minutes, 3 – 4 times per day initially, and then 2 times per day. Apply ice for 15 minutes after any activity to minimize additional inflammation caused by the activity. An ice massage is a very effective form of ice application.
COMPRESSION. This can be achieved by using an ace wrap initially, then by using tape. Then the foot is taped to maintain the arch, and some of the tension on the plantar fascia is relieved.
ELEVATION. Elevating the foot is advised to help reduce swelling, which may be the result of the acute injury or the chronic inflammation.
Night Splint. A night splint holds the plantar fascia and Achilles tendon in a stretch position during sleep. If the fascia is slightly stretched during sleep, then the fascia is spared the sudden stress that occurs with weight-bearing. The night splint will help reduce the pain which occurs with the first few steps in the morning. See the night splint below and additional information in the Sports Med Store.

Medication. An oral anti-inflammatory medication may be prescribed or recommended. If no pain relief has occurred after 2 – 3 weeks, then an injection of cortisone and a local anesthetic into the tender area may be advised. The injection can help relieve the pain and tenderness and make physical therapy more effective. After an injection, the athlete should avoid returning to sports for one to two weeks. A successful injection can often spare the need for surgery. Repeated injections should be avoided.
Exercises. Stretching exercises of the foot and Achilles tendon are essential to help improve muscle tendon flexibility and strength. These exercises help reverse the muscle weakness that results from the inflammation and enable the tendons to resume the usual demands and workloads of the sport (see section on Exercises).
Physical Therapy. This may be necessary to help reduce the inflammation in the plantar fascia. The physical therapist may use such modalities as ultrasound, phonophoresis, iontophoresis, friction massage, electrogalvanic stimulation, and soft tissue mobilization to treat scar tissue in the tendons caused by the chronic inflammation. Later, the small muscles of the foot will be strengthened to support the weakened plantar fascia.
Shoes. Poorly fitting shoes can cause plantar fasciitis. The athlete should select and wear a high-quality running shoe that fits well and has an excellent support. After 300 miles of running in these shoes, expect to lose these supportive features due to significant wear and breakdown. It is wise for a runner to replace his running shoes after 300 miles of wear.
Heel Pads. A heel pad of felt, sponge, or a newer synthetic material can help to spread, equalize, and absorb the shock as the heel lands, reducing the pressure on the plantar fascia. It may be necessary to cut a hole in the heel pad to reduce the irritation to the painful area.

Orthosis and Arch Supports. These devices are either premade or custom-fitted and are inserted into the running shoe, providing support and cushion from the heel and arch to the toes. See the orthotic below and the Superfeet model, with additional information, in the Sports Med Store.

Surgery. Surgery is occasionally required for plantar fasciitis. If all other forms of treatment have failed to provide relief, then surgery should be considered. This usually consists of surgical release of the plantar fascia at the point of greatest tension and removal of heel spurs if necessary.
Returning to Sports
Weight-Bearing vs. Non-Weight-Bearing Sports. Plantar fasciitis can be aggravated by all weight-bearing sports. Any sport where the foot lands and strikes the ground repeatedly, such as running and jogging, can aggravate the problem. Non-weight-bearing sports, such as swimming and cycling, are adequate temporary replacements and can help the athlete maintain cardiovascular fitness without irritating the plantar fasciitis.
Warming Up. The athlete should move all major joints through their complete range of motion several times before starting play. Stretching and strengthening exercises help prevent injury.
Playing the Game. When resuming the sport of choice, play at a lower intensity. In running, run for shorter periods of time, at a slower speed, and less frequently. The athlete should choose flat, even surfaces on which to run. If the athlete experiences pain either during the run or the following morning, then he is doing too much. Resume competitive running or play once the foot has healed.
Exercises
The following exercises are designed to strengthen the small muscles of the foot to help support the injured area. If done regularly, they can help prevent re-injury. Do each prescribed exercise two times a day or more often if necessary.
Towel Curls. Place towel and curl it toward you, using only the toes of your injured foot. Resistance can be increased with a weight on the end of the towel. Relax, then repeat the towel curl. Repeat 15 times, 2 times/day.

Shin Curls. Run your injured foot slowly up and down the shin of your other leg as you try to grab the shin with your toes. A similar exercise can be done curling your toes around a tin can. Repeat 15 times, 2 times/day.

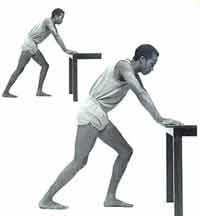
Stretches. Stand at arm's length from a counter or table with your back knee locked and your front knee bent. Slowly lean toward the table, pressing forward until a moderate stretch is felt in the calf muscles of your straight leg. Hold 15 seconds. Keeping both heels on the floor, bend the knee of your straight leg until a moderate stretch is felt in your Achilles tendon. The Achilles tendon attaches the muscles of the calf to the heel bone. Hold 15 seconds more. You should feel a moderate pull in your muscles and tendon, but no pain. Change legs and stretch the other leg. Repeat 15 times, 2 times/day.
I cannot give medical advice about how to treat a specific injury without evaluating the athlete first. While I may discuss general exercises to prevent and treat sports injuries, not all exercises are designed for all individuals or problems. A sports medicine physician should be consulted before starting any exercise program. If an athlete is experiencing any severe pain or discomfort, he should see such a physician and obtain a specific diagnosis and treatment plan. The exercises outlined here are general recommendations and are not intended as a substitute for professional medical advice.
Specialty Reference
Foot & Ankle Center